The following is a case study of a female client, SA, who has a diagnosis of severe learning disabilities, autism and associated communication difficulties. SA is non-verbal and communicates through objects of reference, body language and challenging behaviour, in the form of self-injury behaviour or aggression to others. Some of the challenging behaviours include banging her head, biting and scratching areas of her body, hitting, biting and hair pulling and or head butting others. A pattern emerged over time where the reduction in one form of self-injury behaviour was often replaced by other high-risk behaviours (e.g. acrobatics). SA experiences periods of extremely distressed and unsettled behaviour- defined as amber and red arousal states. These periods last from a few hours to a couple of days, followed by a period of time when SA is settled.
At times over the last twelve years, these periods would sustain for up to several months, with little respite from her distress. Numerous investigations into possible underlying health issues were undertaken but no problems were ever identified which would explain the situation. The close supervision often needed to support SA in all her activities e.g. personal care, eating and drinking, and bathing after frequent smearing behaviour meant that she experienced regular demands throughout the day, which resulted in challenging behaviour that subsequently reduced the opportunities for positive staff interactions.
Despite these challenging episodes, SA is still very sociable, and one of her strengths is her ability to develop close and lasting relationships with co-workers. Close contact with and support from co-workers is extremely important to SA but during extended periods of challenging behaviour, these relationships came under severe stress. Despite these challenges, the whole team of co-workers would persevere in working with her and tried to work out why SA was feeling so distressed.
In June 2015, SA’s presentation suddenly deteriorated, and she exhibited a high level of self-injury behaviour (biting herself and banging her head on hard surfaces) and aggression directed at others. Due to the high frequency and severity of presented behaviours, she was referred to Learning Disability Team and Intensive Support Team. Both teams, carried out extensive work (functional assessment of challenging behaviour including observation, staff systematic sessions, communication assessment and medical investigations, including dental treatment, and blood test undertaken under general anaesthetic) to find causes of the sudden onset of the self-injury behaviour. No new information about the causes or functions of SA’s stressed behaviours was identified during this process, although it was already understood that her stress was linked to communication needs, attention and interaction.
New strategies were implemented by the positive support co-ordinator and teams at home to reduce the level of SA’s anxiety such as the small circle of support (only a few co-workers were supporting SA), changes in the environment (she moved from the main building, which she shared with 5 other service users, to annex in the garden). In addition, medical interventions (Olanzapine) were applied. New strategies reduced SA’s self-injury behaviour but aggression directed at others remains on the same level.
The change of living area for SA was accompanied by a reduction in the SIB as she was able to spend time away from noisy and unpredictable environments, but her stress remained high whenever she saw non-preferred co-workers.
During this period, work was also done by the teams to identify the key characteristics of the co-workers that SA would accept, which included a calm, quiet demeanour and an ability to support SA at her own pace and without a perception of demands. Being highly responsive and supporting SA to take the lead proved a successful approach when carried out by this small team, and challenging behaviours gradually reduced.
Small circle of co-workers, who worked with SA over last 18 months. From left: Alex, Emma, Katy, Zoe, Lorraine (behind), Diana, Maria and Emma B (not at the picture)
In May 2016, co-workers received extensive Intensive Interaction training from Mr Jules McKim from Southern Health NHS Foundation Trust. The aim of the training was to encourage staff to interact at an appropriate developmental level for SA and to demonstrate to SA that interactions are not all demands based, and to provide her with opportunities to learn fundamental communication skills and enjoy her time with others.
After the intensive interaction training, there were three scheduled follow-up meetings with Mr McKim, where co-workers were able to reflect and discuss what was working. Intensive Interaction session recording forms and videos of SA and co-workers were available for review and discussion, where different intensive interaction techniques were discussed. During the second meeting in December 2016, coworkers reported that interactions with SA were ‘amazing’ and SA is more seeking out face-to-face contact and interactions. At this time SA was still supported by a small core team of female co-workers with whom she had close and trusting relationships, but would also by now seek out and accept support from less preferred co-workers in the wider teams. The last follow-up meeting took place in February 2017, where co-workers again shared their experiences and how they felt about intensive interactions. Here are a few quotes from the session and Intensive interaction session recording forms:
‘I am happy that I and SA had a good session… that SA led the session.’
‘Really happy and proud that SA was laughing and looked so relaxed’
Katy
‘Staff were happy as she allowed them to interact with her…even for the staff she targets.’
Maria
‘I felt happy seeing her calm and change in her behaviour’
Lorraine
Since co-workers have been using the Intensive Interactions approach, SA learned that interactions did not have to be based on demands and she gained control over interactions and to a lesser extent, the environment. Currently, she presents herself in a calm and settled mood with occasional days where is more anxious, but the level of challenging behaviour directed at others is much less frequent and severe.
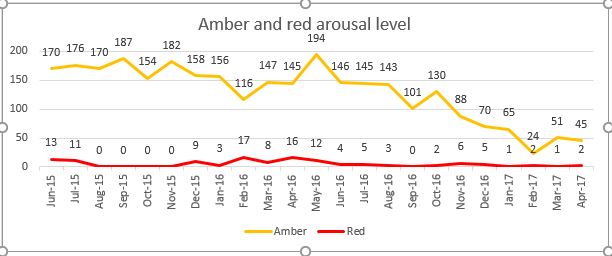
Figure 1, shows SA’s arousal level from June 2015 to April 2017. Amber’s arousal level- unsettled, anxious not able to participate in offered activities, red arousal level- distressed, highly anxious.
Katarzyna Kowalska
Positive Support Coordinator